Active surveillance for prostate cancer has its tradeoffs. Available to men with low- and intermediate-risk prostate cancer, the process entails monitoring a man’s tumor with periodic biopsies and prostate-specific antigen (PSA) tests, and treating only when — or if — the disease shows signs of progression.
Active surveillance allows men to avoid (at least for a while) the side effects of invasive therapies such as surgery or radiation, but men often feel anxious wondering about the state of their cancer as they spend more time untreated. Is there a middle path between not treating the cancer at all and aggressive therapies that might have lasting side effects? Emerging evidence suggests the answer might be yes.
During a newly-published phase 2 clinical trial, researchers evaluated whether a drug called enzalutamide might delay cancer progression among men on active surveillance. Enzalutamide interferes with testosterone, a hormone that drives prostate tumors to grow and spread. Unlike other therapies that block synthesis of the hormone, enzalutamide prevents testosterone from interacting with its cellular receptor.
A total of 227 men were enrolled in the study. The investigators randomized half of them to a year of daily enzalutamide treatment plus active surveillance, and the other half to active surveillance only. After approximately two years of follow-up, the investigators compared findings from the two groups.
The results showed benefits from enzalutamide treatment. Specifically, tumor biopsies revealed evidence of cancer progression in 32 of the treated men, compared to 42 men who did not get the drug. The odds of finding no cancer in at least some biopsy samples were 3.5 times higher in the enzalutamide-treated men. And it took six months longer for PSA levels to rise (suggesting the cancer is growing) in the treated men, compared to men who stayed on active surveillance only.
Enzalutamide was generally well tolerated. The most common side effects were fatigue and breast enlargement, both of which are reversible when men go off treatment.
In an accompanying editorial, Susan Halabi, a statistician who specializes in prostate cancer at Duke University, described the data as encouraging. But Halabi also sounded a cautionary note. Importantly, differences between the two groups were evident only during the first year of follow-up. By the end of the second year, signs of progression in the treated and untreated groups “tended to be very similar,” she wrote, suggesting that enzalutamide is beneficial only for as long as men stay on the drug. Longer studies lasting a decade or more, Halabi added, may be necessary to determine if early enzalutamide therapy changes the course of the disease, such that the need for more invasive treatments among some men can be delayed or prevented.
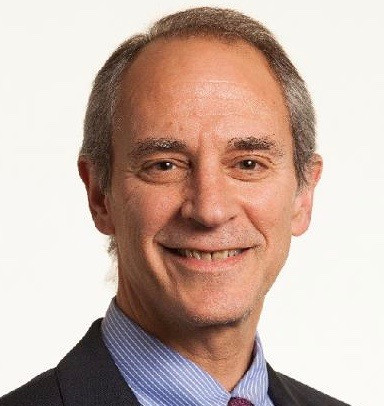
Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, editor of the Harvard Health Publishing Annual Report on Prostate Diseases, and editor in chief of HarvardProstateKnowledge.org, said the study points to a new way of approaching active surveillance, either with enzalutamide or perhaps other drugs. “An option that further decreases the likelihood that men on active surveillance will need radiation or surgery is important to consider,” he says. “This was a pilot study, and now we need longer-term research.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt